Trachomatous trichiasis, a condition where inward-turned eyelashes scratch the surface of the eye and can lead to blindness, can be effectively treated through two common surgical techniques, according to a new study funded by the National Institutes of Health (NIH). This research, published in PLOS Neglected Tropical Diseases and supported by the National Eye Institute (NEI), provides reassurance about the effectiveness of existing surgical methods.
Previous smaller studies suggested that one surgical technique might yield poorer outcomes, leading to concerns among healthcare providers. “Some studies have reported post-operative trichiasis rates of 30% or higher,” said Emily Gower, Ph.D., from the University of North Carolina at Chapel Hill. “This trial aimed to see if we could reduce the risk of post-operative trichiasis by modifying surgical procedures. Our findings indicate that existing methods provide better outcomes than previously thought.”
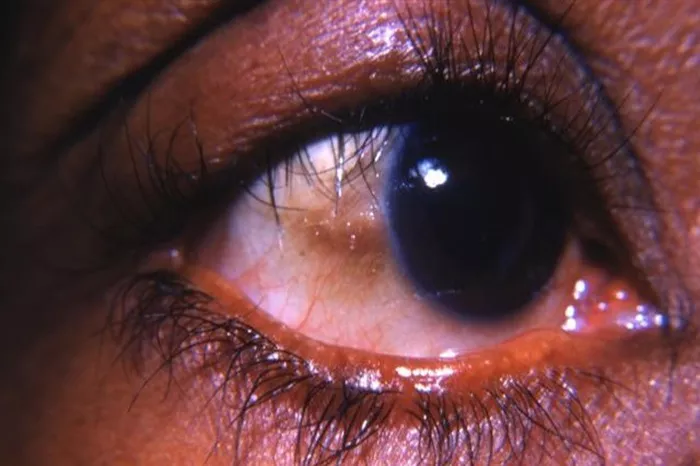
Globally, approximately 1.7 million individuals, predominantly in impoverished rural regions of Africa, are affected by trachomatous trichiasis. The condition typically results from chronic infections with the bacterium Chlamydia trachomatis, which spreads through direct person-to-person contact. Trachoma is particularly prevalent in hot, dry climates, and repeated infections can lead to scarring that forces the eyelid to turn inward, causing the eyelashes to irritate the eye. If untreated, trichiasis can lead to corneal clouding and eventually blindness.
Surgery remains the most common and effective treatment for trichiasis, aimed at correcting the eyelid’s inward turn. There are two primary surgical methods: posterior lamellar tarsal rotation (PLTR) and bilamellar tarsal rotation (BLTR). Prior studies had suggested that PLTR might be more effective, prompting some African programs to retrain surgeons in this technique. Additionally, previous analyses indicated that adjusting the incision placement for BLTR—5 mm above the eyelid margin rather than the standard 3 mm—could potentially reduce recurrence rates, although this modification had not been rigorously tested.
The current study, conducted in southern Ethiopia, enrolled 4,914 patients with trichiasis in one or both eyes, resulting in a total of 6,940 eligible eyes. Participants were randomly assigned to receive either BLTR with a 3 mm incision, BLTR with a 5 mm incision, or PLTR. Follow-up assessments for post-operative trichiasis were conducted at six weeks and again at 12-18 months after surgery. On average, about 17% of eyelids experienced post-operative trichiasis. The study found no significant difference in post-operative trichiasis rates between the two methods using a 3 mm incision. However, those treated with the 5 mm BLTR were significantly more likely to experience post-operative issues.
The results suggest that the standard surgical techniques—either BLTR or PLTR at a 3 mm incision height—are preferable for treating trichiasis, underscoring their effectiveness in preventing recurrences and promoting better patient outcomes.
Related topic:
Eva Mendes’s Beauty Secret: The Must-Have Concealer for Dark Circles
How Is Lower Blepharoplasty Done?